What is A1C?
A1C estimates a person’s average blood sugar levels over a 2- to 3-month span, and is usually measured in a doctor’s office or in a lab with routine blood work. Sometimes called HbA1c, hemoglobin A1C, or glycated hemoglobin, it is one standard measure of blood glucose (or blood sugar).
How does A1C work?
A1C testing uses hemoglobin, the part of the red blood cell that carries oxygen throughout the body. Glucose in the blood sticks to hemoglobin, and the more glucose in your blood, the more that sticks! That glucose can stay there for around three months—about how long the average red blood cell lives. A1C test results are reported as a percentage. The higher the percentage, the higher your blood glucose levels over the past two to three months.
Since the A1C test can measure average glucose levels over a period of time, it can be helpful for determining your risk of diabetes-related complications. For example, a lower A1C is correlated with a lower risk of microvascular complications, such as kidney disease, vision loss (retinopathy), and nerve damage. Similarly, a consistently high A1C can lead to macrovascular complications like heart disease.
Want this information sent straight to you?
Sign up for free to get diabetes information sent straight to your inbox once a month.
How to interpret your A1C
Your A1C can help identify whether you have or are at risk for prediabetes or diabetes, as well as monitor your management if you already live with diabetes.
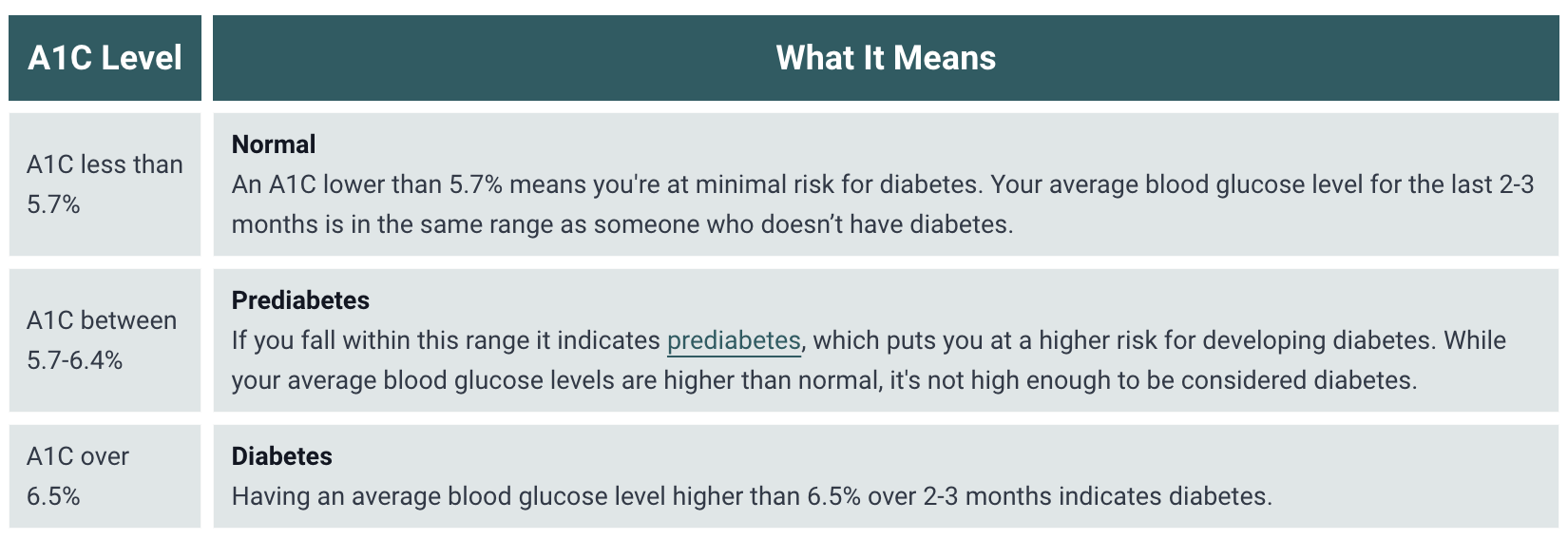
Estimated average glucose (or eAG) can tell you your average blood sugar based on your A1C (HbA1c) result:
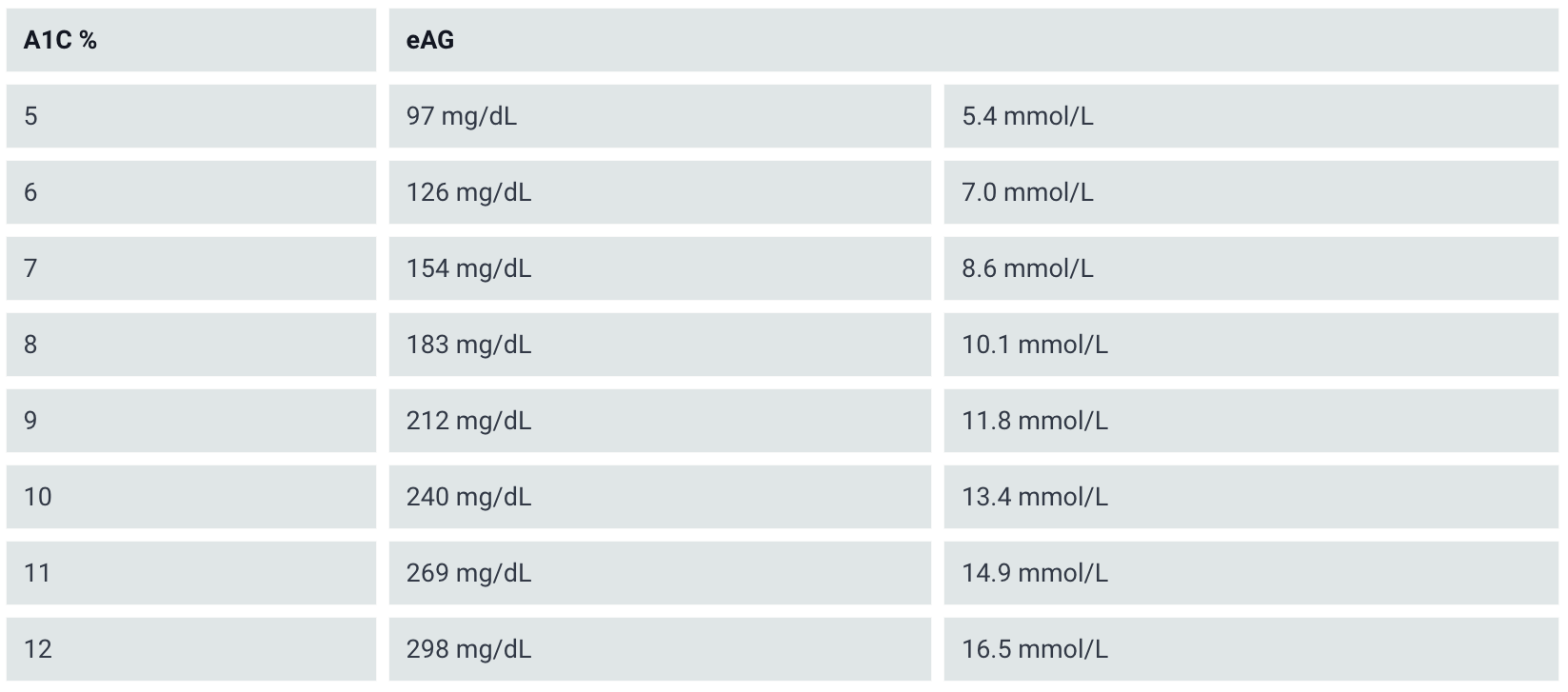
According to the American Diabetes Association’s 2024 Standards of Care, A1C goals should be individualized based on a number of factors. However, the A1C goal for most nonpregnant adults is <7% (<53 mmol/mol). Your diabetes care team can help identify the best target A1C for you.
Limitations of A1C
While A1C can be a helpful tool, it’s important to know that accuracy may be affected by a variety of factors like medications and supplements, medical conditions, age, and genetics, including hemoglobin variants that lead to varying accuracy across racial and ethnic groups.
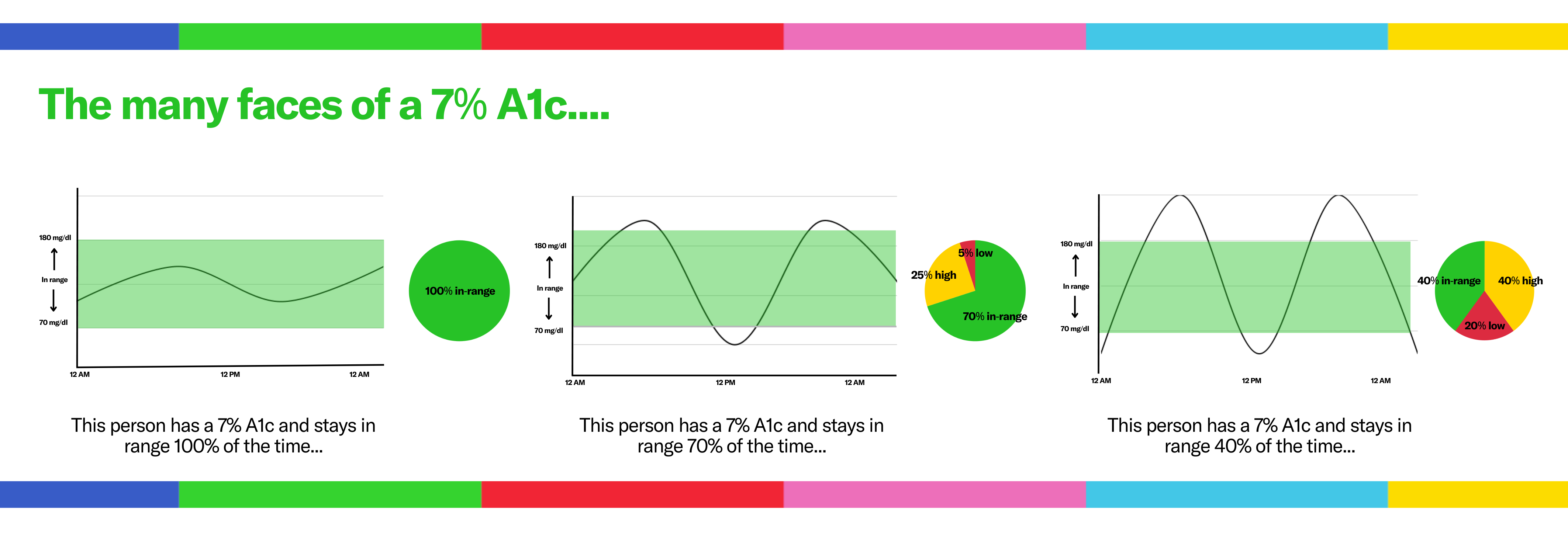
Most importantly, remember that your A1C is just a number and is not a grade or indication of whether you’re living a healthy life. As an average, A1C (HbA1c) cannot capture critical information such as how high or low your glucose levels go. You could have the same A1C as someone else, but feel different because you’re spending more time high or low. To better understand these nuances, we use time in range.
What is Time in Range (TIR)?
Ultimately, time in range shows you the ENTIRE picture. Time in range (TIR) is the percentage of time that a person spends with their blood glucose levels in a target range. When we refer to TIR, we also mean the metrics that are measured along side it—like time below range (TBR) and time above range (TAR).
Time in range is usually measured through a continuous glucose monitor (CGM), and captures the highs (hypoglycemia), lows (hyperglycemia), and in-range values that characterize daily life with diabetes. Using time in range to manage your diabetes can help you recognize patterns and learn what works best for your body and your life — like how your glucose responds to changes in your food, exercise, sleep, hormones, and so much more.
Like A1C, the target range will vary depending on the person, but for most people, guidelines suggest starting with a range of 70 to 180 mg/dL, with the goal of spending at least 70% of your time in range, less than 4% of your time below range, and less than 1% of time very low, or below 54 mg/dL (3 mmol/L).
Using time in range alongside A1C (HbA1c) can empower you to learn your glucose patterns in between appointments with your care team, and can facilitate more informed decision-making with your doctor. There are over 42 factors that can cause blood sugar to levels to increase and decrease, and using time in range can help you identify those factors and make changes. You can see what foods raise your blood sugar, what can help you lower blood sugar, and so much more.
Maybe your A1C is on target, but you’re really struggling with post-meal highs and re-bound lows—time in range can help you and your care team adjust your management to help you feel better, faster.
If you’re interested in learning more about time in range and how you can get started, sign up for our free monthly newsletter here!