Started
GETTING STARTED WITH TIME IN RANGE



















Getting started with a CGM
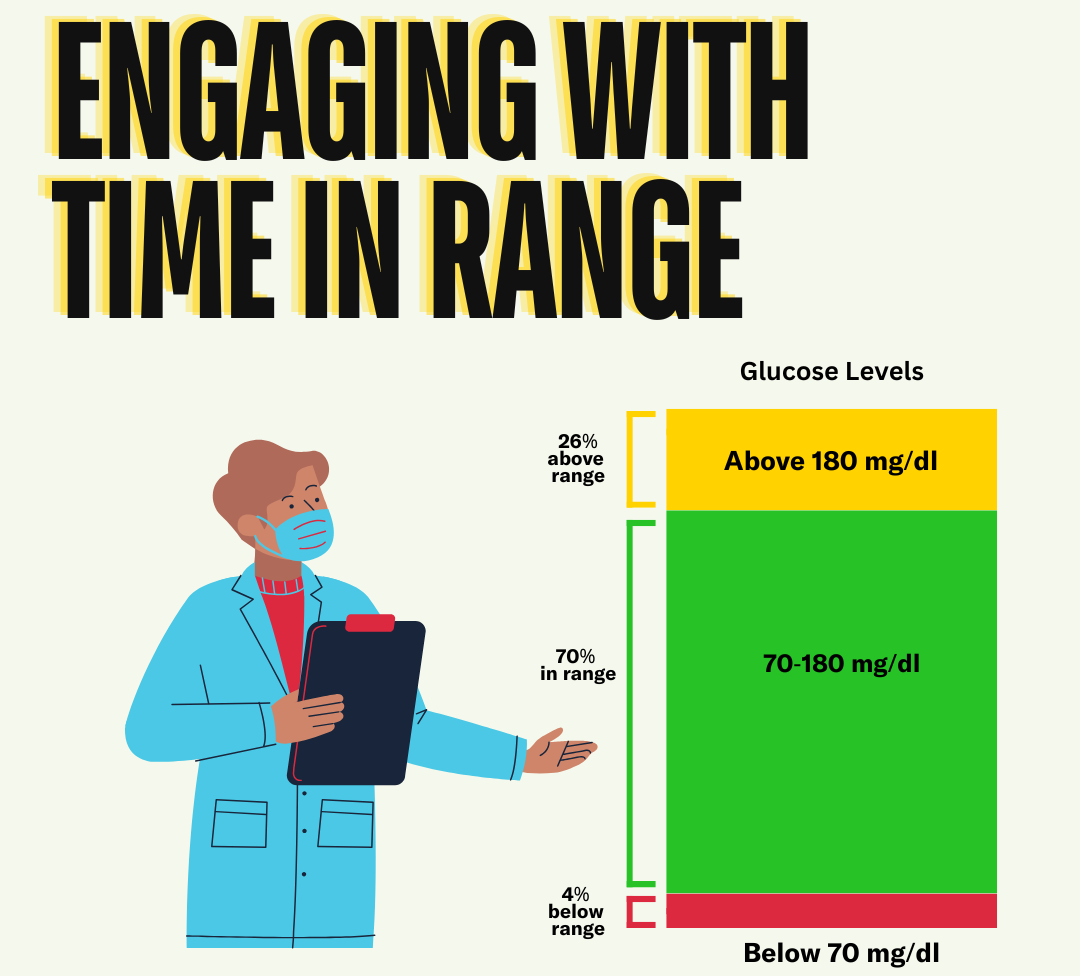
CGM is used by persons with diabetes to make treatment decisions in day to day diabetes management. It’s a great diabetes management tool because CGM provides a value of glucose, but also a trend arrow that indicates speed and direction of change of glucose. CGM can be used to calculate time in range in daily, weekly or longer periods of time to help identify patterns of glucose to make treatment decisions including medication adjustments or additions.
CGM has been shown to improve one’s diabetes management for people with type 1 and type 2 diabetes. Many people do not have access to these life changing devices largely due to awareness, cost, and racial bias in the healthcare system. However, there’s work being done every day to increase access for everyone with diabetes, and Medicare has expanded CGM coverage to include people using any sort of insulin.
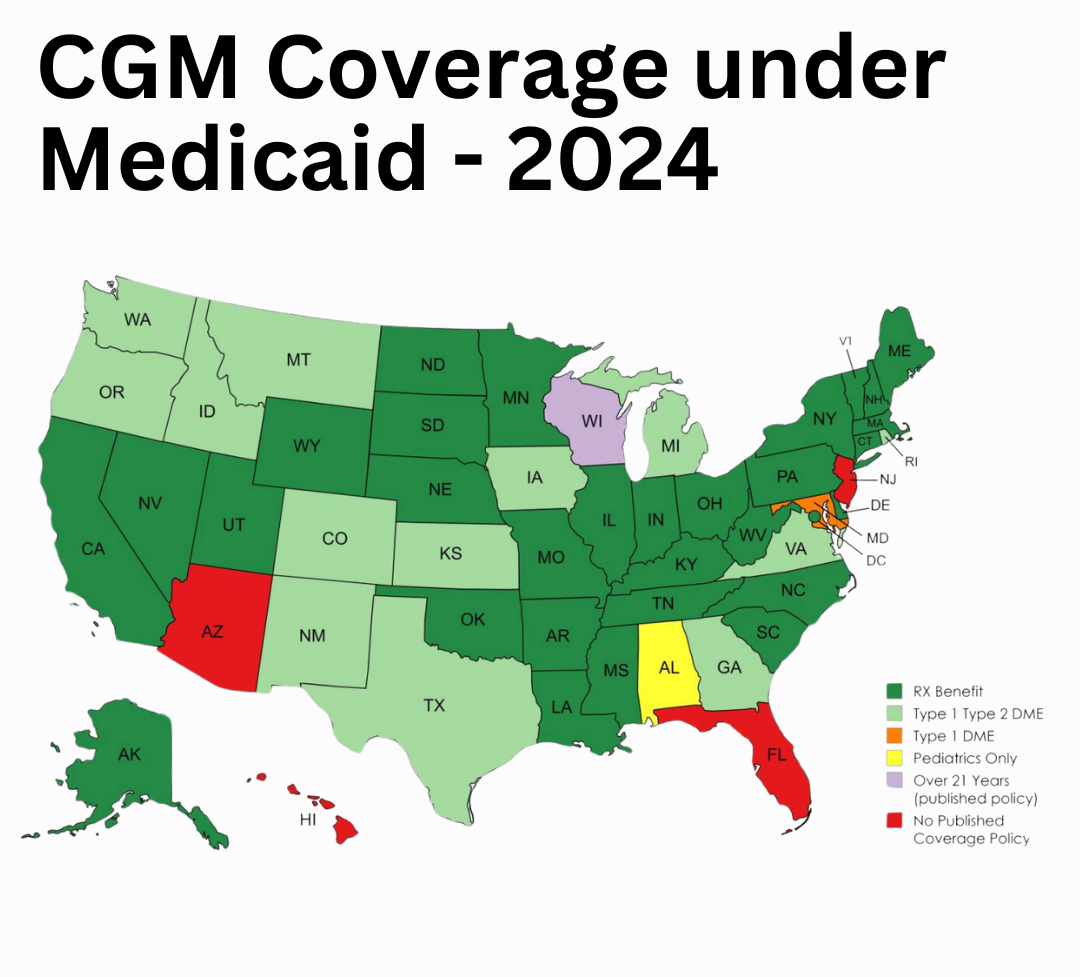
Over 7 million people with diabetes in the US rely on insulin—and so far, 25% of them use a CGM. A few of the main drivers of CGM access disparities include: knowledge about CGM and TIR, insurance coverage, and bias among healthcare providers. We hope to address a few of the main drivers of CGM access disparities (knowledge about CGM and TIR, insurance coverage, and bias among healthcare providers) and increase adoption of CGM and TIR through education and advocacy efforts.Increased insurance coverage from the Affordable Care Act and the expansion of Medicaid to more states allows more people with diabetes to use insulin pens, pumps, and CGM. Most recently, the centers for Medicare and Medicaid Services (CMS) updated their coverage policy to include more people with type 2 diabetes.
CGMs require three basic parts:
- A sensor that monitors real-time glucose levels under your skin.
- A transmitter that sits on top of the sensor and sends glucose information to a smartphone app, reader, or receiver. In transcutaneous systems, the sensor and transmitter are connected as one small on-body device. Some transmitters are disposable with the sensor while others require an additional step to attach. In implanted systems, the transmitter is attached to the skin and can be removed without harming the sensor below the skin.
- A smartphone app, reader or receiver to collect and display your data
CGMs have a variety of features that differ by brand and model, including the amount of time the CGM needs to “warm up” before glucose readings are available, how long you can wear a sensor before needing to replace it, and alarms that alert you to highs and lows.
You can use this website to compare different CGM devices.
CGMs can be covered by insurance providers, through pharmacy benefits, and patient savings programs. You should stay in touch with your company representatives about what has changed because coverage can change rapidly.
Danatech is a tool that allows one to check insurance coverage for CGM by device type, state, and insurance plan.
Some people may not have insurance or even if they do, it may not be enough to cover the costs of a CGM. Fortunately, there are CGM insurance and affordability programs that can help with the cost. You can find a list of them here.
Prescribing a CGM will vary by whether it’s a personal or professional device.
Here is more information on how to prescribe a CGM by device type:
Latest Research
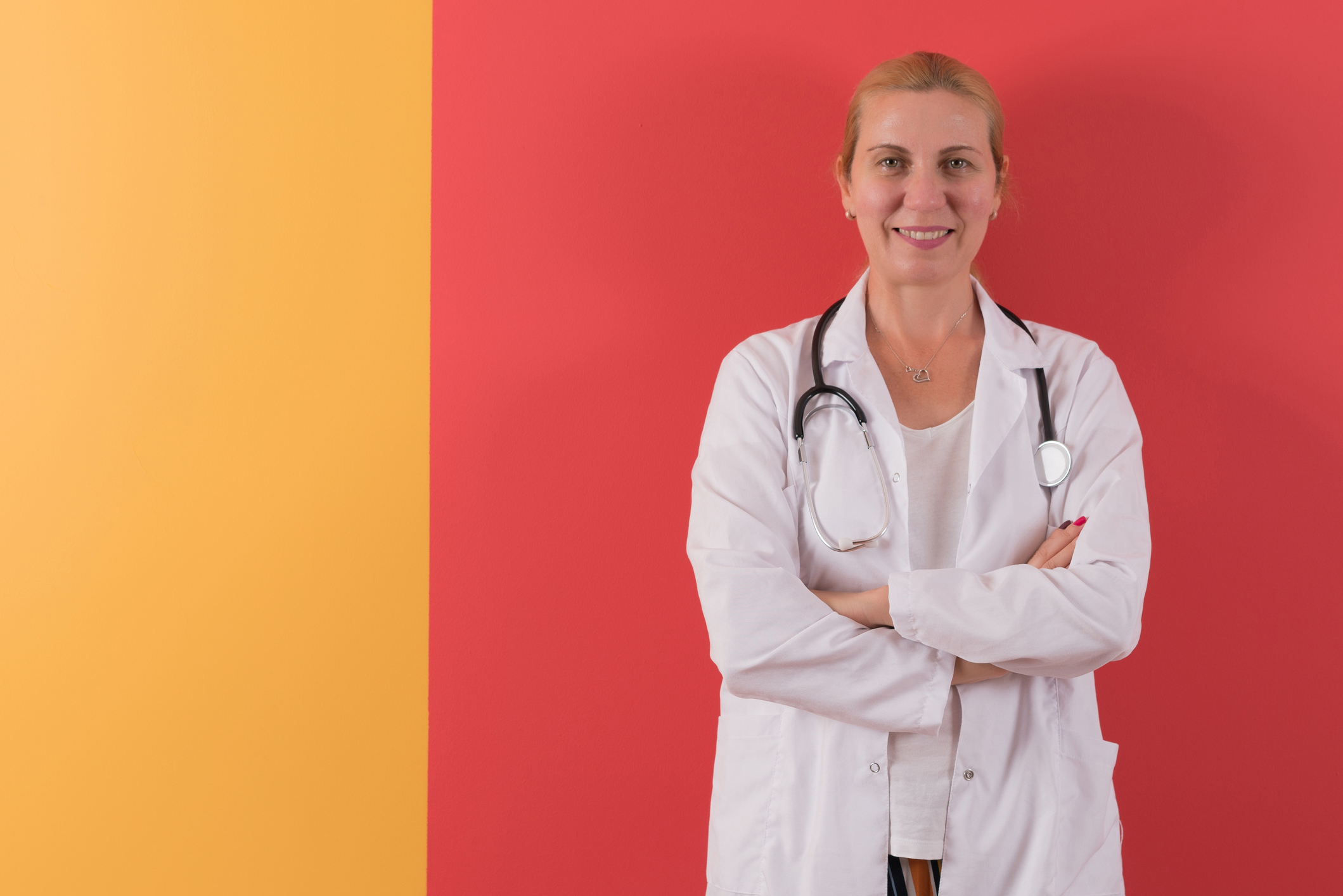
Health Care Providers
Topic
-
Awareness of Time in Range – Opportunities for Increased AdoptionThese data highlight a significant lack of TIR awareness among people with T2 and CGM non-users....
-
Utilization of Time in Range in Real World Varies by Type of DiabetesGreater access to CGMs may enable more people with diabetes to use TIR in their daily disease management....
-
Awareness of Time in Range Varies by Type of Health Care ProviderThis data highlights a significant lack of TIR awareness among PCPs as compared to DEs and Endos...
-
CGM Access is the Main Barrier to TIR Use Among ProvidersThese data highlight a lack of access to CGM as a key barrier to the adoption and use of TIR among HCPs...