When managing your diabetes, you want the most accurate information possible! with advancements in diabetes technologies that provide immediate and accurate metrics, why are healthcare offices still using data that could be inaccurate?
Hemoglobin A1C (HbA1c or “A1C”) is the metric most often used in healthcare offices, but it can be inaccurate for certain groups and medical conditions. An A1C test measures how much hemoglobin (an important component of red blood cells) has sugar attached to it. Once a red blood cell becomes coated with sugar, the sugar stays there for 2-3 months (this is why you get your A1C tested every 3 months). A1C results can be impacted because of the rate of red blood cell turnover —which means it’s not accurately measuring how much sugar is attached to the blood cells.
See if you fall into one of the groups that often see inaccurate A1C results:
People of color
Studies show that A1C values are less accurate for people of African, Mediterranean, or Southeast Asian descent.
Specifically, A1C has been shown to frequently overestimate glucose levels in African American individuals. Genetic variants can also cause hemoglobinopathies, a group of blood disorders and diseases that affect red blood cells—which can affect A1C results, as the A1C test does not account for these differences in hemoglobin.
As a result, A1C standards may be inaccurate for some. When you’re working with your healthcare team to make changes in your routine and management, you want the most accurate information possible! Talk to your healthcare team if you’re worried about your A1C being inaccurate and check out our resources for getting started on a CGM to avoid these issues.
Older Individuals
As people age, we are more susceptible to red-blood cell turnover rate changes. Older populations have a higher risk of conditions that affect these rate changes—things like iron deficiency (anemia), dialysis, sickle cell anemia, recent blood transfusions, and more. This can affect A1C results and make them inaccurate, either higher or lower than the actual average blood glucose.
A1C also does not show low glucose patterns which is extremely important to monitor in older individuals, as low glucose can lead to injuries or cognitive issues—something we all want to avoid!
Solely using A1C in diabetes management could increase hypoglycemia risk in older people with diabetes—meaning more hospital visits and potentially dangerous situations. For older adults, CGM should be used for daily diabetes management, as CGM metrics like time in range (TIR) can provide accurate insights into the WHOLE picture of diabetes. A complete picture means less stress, a better ability to manage glucose, and more opportunities to enjoy your days.
People with kidney disease
Research shows that A1C may be less accurate for people with chronic kidney disease (CKD), especially those with advanced CKD.
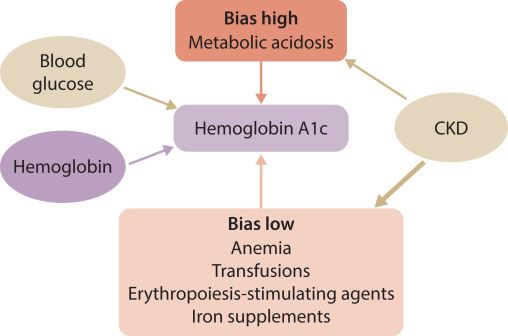
Common CKD comorbidities and treatments, including anemia, blood transfusions, iron supplements, and erythropoiesis-stimulating agents, can result in a lower A1C, while metabolic acidosis can result in a higher A1C.
Image: Effects of chronic kidney disease (CKD)–related factors on glycated hemoglobin (HbA1c).
As A1C is measured by the red blood cell life span, when the kidneys begin to fail, they are unable to remove acids that build up in the body. This buildup of acids (metabolic acidosis) speeds up the process of sugar binding to the red blood cell, causing A1C to appear to be higher—as the red blood cells’ life span becomes shorter.
Comorbidities like anemia and treatments like blood transfusions and CKD medications can reduce red blood cell production, meaning there are less blood cells for the sugar to bind to, resulting in a lower A1C.
Kidney Disease: Improving Global Outcomes (KDIGO) global guidelines encourage CGM use in people with CKD. Recent evidence has shown that increasing time in range can lower risk of kidney damage in people with type 1 and type 2 diabetes!
Time in range and CGM can give an accurate picture of a person’s management with CKD—and it can be a more accurate indicator of the risk of complications across the board, as well as a powerful tool for you to understand your diabetes on a deeper level, right from the palm of your hand.
Pregnant Individuals
There is conflicting evidence on whether pregnancy overestimates or underestimates A1C—but we know that pregnancy is a factor in creating inconsistent and inaccurate A1C test results.
Similarly to aging populations, pregnancy changes the life-cycle of the red blood cell, which can affect A1C. It’s also been found that using A1C could provide false reassurance if it’s used to measure glucose levels in mid- to late-gestation.
Diabetes management is important for fetal development—inaccurate measurements of A1C can be serious. It’s vital to be able to not only get an accurate measure of glucose levels, but a full picture. A1C doesn’t capture swings in glucose and misses the opportunity to provide actionable insights into daily management—using a CGM and time in range can give pregnant individuals the clarity to know exactly where their levels are, protecting themselves and their baby!
Alternatives to A1C
Continuous glucose monitoring (CGM) provides accurate glucose levels and metrics that show the entire picture of your diabetes management—with readings every 5 minutes, you don’t have to play guessing games every three months.
Time in range shows the average percentage of time someone spends within their target range of 70-180 mg/dl, time below range (<70 mg/dl, TBR), and time above range (>180 mg/dl, TAR) and it provides this information daily, weekly, monthly and quarterly This allows you and your healthcare team to see the full picture—and work together to manage your diabetes in the way that works for you.
Click here to learn more about how time in range can help you thrive!

